The medical imaging workflow is the intricate choreography of modern diagnostics—a sophisticated process that begins with a clinical question and culminates in a report that shapes a patient’s future. This is not a mere sequence of administrative tasks; it is a high-stakes operational ballet involving advanced technology, clinical expertise, and seamless data exchange. Mastering this workflow is no longer an operational goal; it is a strategic imperative for any healthcare organization dedicated to delivering timely, precise, and life-saving care.
Deconstructing the Diagnostic Engine

At its core, the medical imaging workflow is the central nervous system of diagnostics. It transcends technical protocols to become a strategic logistics operation, where every handoff—from the referring physician to the technologist, from the PACS administrator to the radiologist—must be executed with flawless precision.
This critical pathway orchestrates the efforts of every stakeholder: the clinician seeking diagnostic clarity, the administrative team managing complex schedules, the technologist capturing pristine images, and the radiologist synthesizing data into a definitive clinical narrative. The ultimate purpose is to transform a diagnostic uncertainty into an actionable, evidence-based answer.
Why Optimization Is a Clinical Imperative
An inefficient, fragmented workflow introduces dangerous friction into the care continuum. Bottlenecks in scheduling, sluggish image transfers, or reporting backlogs are not just operational hurdles—they represent postponed diagnoses and delayed interventions that directly compromise patient outcomes.
Conversely, a highly optimized, intelligent workflow accelerates decision-making, mitigates the risk of diagnostic error, and alleviates the mounting pressures on clinical staff.
This optimization is paramount as demand escalates. The global medical imaging market reached USD 41.6 billion in 2024 and continues its upward trajectory. This growth is largely fueled by demographic shifts; the UN projects the global population over 65 will surge to 1.6 billion by 2050, intensifying the need for rapid, reliable diagnostic services.
At its core, optimizing the medical imaging workflow isn't about moving images faster. It's about accelerating the speed of accurate diagnosis, which is the true currency of effective healthcare.
To fully grasp this ecosystem, let's dissect its foundational stages.
Core Stages of the Medical Imaging Workflow
| Stage | Key Action | Primary Goal |
|---|---|---|
| 1. Order & Scheduling | A physician orders a scan, and the patient is scheduled for an appointment. | To capture clinical intent and orchestrate the exam logistics. |
| 2. Image Acquisition | A technologist performs the scan (MRI, CT, etc.) and captures the images. | To generate high-fidelity, diagnostically valuable image data. |
| 3. Image Interpretation | A radiologist analyzes the images to identify findings and abnormalities. | To translate visual data into a cogent medical diagnosis. |
| 4. Reporting & Delivery | The radiologist creates a formal report, which is sent back to the referring physician. | To communicate diagnostic insights clearly and guide clinical action. |
| 5. Archiving & Follow-up | Images and reports are stored securely for future reference and comparison. | To maintain a longitudinal patient record and ensure compliance. |
Each stage is a critical link, dependent on the integrity and efficiency of the preceding one.
The Key Players in the Workflow
A successful diagnostic journey is the product of a multidisciplinary team operating in perfect synergy. Understanding these roles is essential to appreciating the workflow's complexity.
- Referring Physicians: They initiate the diagnostic process, identifying the clinical need for an imaging study based on patient presentation.
- Technologists: These are the technical experts who operate sophisticated imaging modalities—MRI, CT, X-ray—to acquire images of the highest diagnostic quality.
- Radiologists: As specialist physicians, they are the interpreters of diagnostic data, responsible for analyzing images, identifying pathology, and authoring the definitive report.
- IT and Admin Teams: The operational backbone, managing the complex software infrastructure like PACS (Picture Archiving and Communication System) and RIS (Radiology Information System) that facilitates data flow and ensures operational integrity.
Understanding how these roles intersect with the underlying healthcare technologies is the first step toward building a truly world-class diagnostic capability.
Navigating the Five Core Stages of Image Management
To truly master the medical imaging workflow, one must trace the journey of a diagnostic image from inception to clinical action. This is not a single event but a sequence of five distinct, interdependent stages. Think of it as a strategic relay, where technological sophistication and human expertise must align to seamlessly pass the baton from one phase to the next.
This journey begins not with a scan, but with a clinical question demanding an answer.
Stage 1: Order Entry and Scheduling
The workflow commences when a referring physician places an order for an imaging study. This foundational step is critical; inaccuracies or incomplete information here can create cascading inefficiencies downstream. The order must articulate the patient's clinical context and the precise diagnostic question, as this informs the entire subsequent process.
From there, scheduling teams must align patient availability with the appropriate equipment and personnel. Modern Radiology Information Systems (RIS) are indispensable here, enabling optimized scheduling, automated patient communication, and clear preparatory instructions. A well-executed scheduling process minimizes no-shows and ensures the technologist is fully equipped with the necessary clinical context.
Stage 2: Image Acquisition
This is the moment of data creation. A highly skilled technologist confirms patient identity, explains the procedure, and precisely positions the patient. The primary objective is to acquire diagnostically superior images while prioritizing patient safety, such as adhering to the ALARA (As Low As Reasonably Achievable) principle for radiation dosage in CT scans.
Success at this stage hinges on protocol optimization—employing imaging parameters tailored to the specific clinical inquiry. A protocol for acute stroke evaluation, for instance, is vastly different from one designed for a musculoskeletal injury. Standardizing these protocols ensures consistent, high-quality outcomes across an entire health system, regardless of the technologist on duty.
The infographic below illustrates the time-critical nature of the subsequent stages following image acquisition.
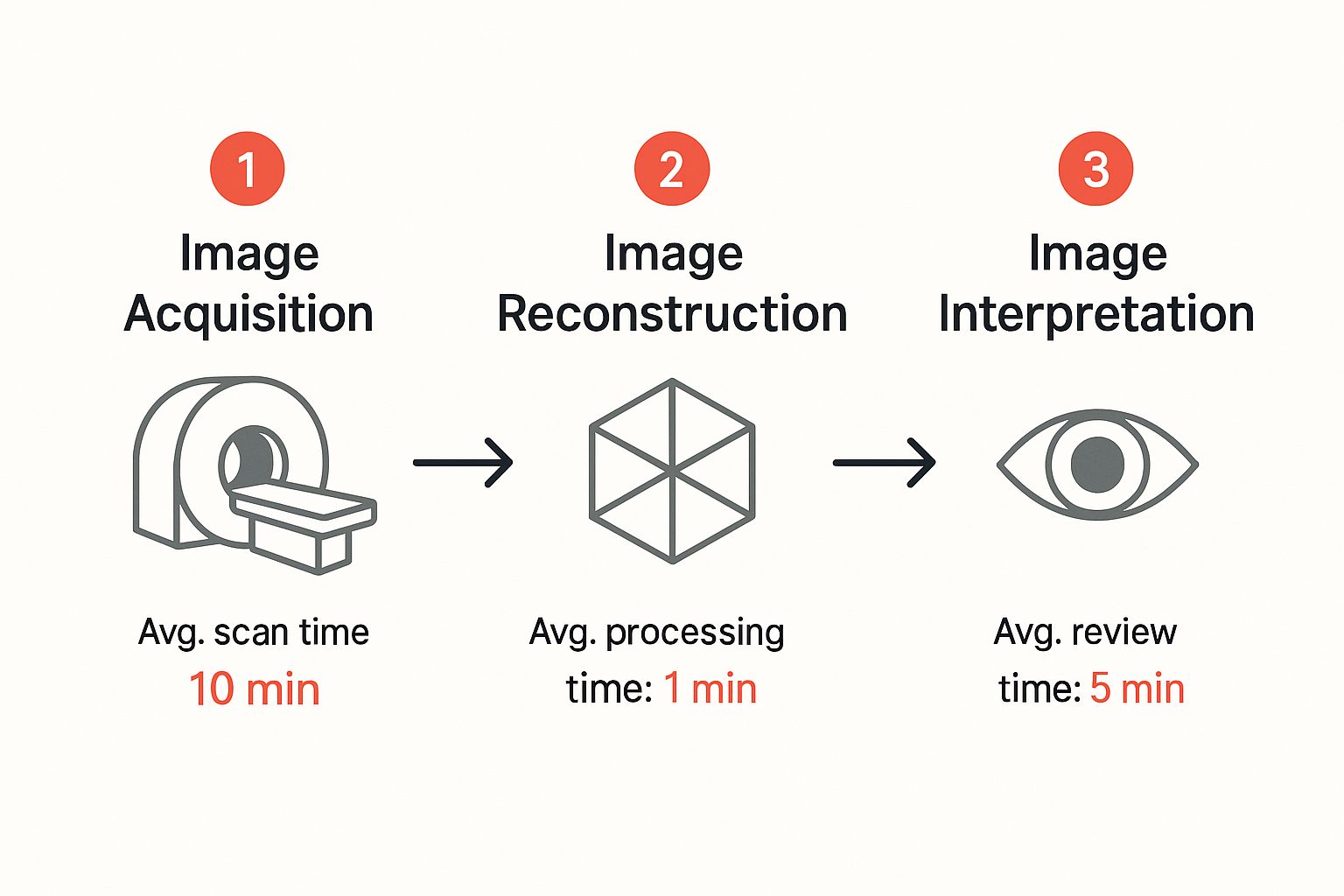
This visual underscores that a standard 10-minute scan is merely the beginning of a multi-step process requiring further processing and expert analysis before a diagnosis is rendered.
Stage 3: Processing and Archiving in PACS
Immediately post-acquisition, raw image data is transmitted to the Picture Archiving and Communication System (PACS). This is the digital epicenter of radiology—a secure, robust repository that stores, retrieves, and displays all medical images.
Here, images may undergo post-processing, such as the creation of 3D reconstructions from CT data sets. The PACS then archives the images, meticulously linking them to the correct patient record. For the medical imaging workflow to function as a cohesive unit, the RIS and PACS must be flawlessly integrated, ensuring perfect alignment between patient data and imaging studies.
A well-integrated RIS/PACS ecosystem serves as the single source of truth, dismantling the data silos that breed inefficiency and risk. It provides the radiologist with a comprehensive, contextualized view of the patient's case.
Stage 4: Radiologist Interpretation and Reporting
This is the cognitive core of the workflow. A radiologist—a physician with extensive subspecialty training—retrieves images from the PACS for analysis on a high-resolution diagnostic monitor. They compare new studies with prior imaging to assess disease progression, identify abnormalities, and formulate a diagnosis.
The radiologist then authors a structured report containing:
- Technique: A concise summary of the imaging protocol.
- Findings: An objective, detailed description of observations within the images.
- Impression: The definitive diagnosis or differential diagnoses, directly addressing the referring physician's clinical question.
Modern innovations, including voice recognition and structured reporting templates, are accelerating this stage while enhancing the clarity and consistency of the final report.
Stage 5: Results Distribution
The final stage involves delivering the diagnostic report to the referring physician to inform clinical decision-making. This is more than a simple file transfer; it is a closed-loop communication system designed for speed and security.
Results are typically integrated directly into the facility's Electronic Health Record (EHR), ensuring immediate accessibility. For critical or unexpected findings, established protocols mandate direct communication—often a radiologist-to-physician phone call—to ensure patient safety is never compromised. Closing this loop effectively completes the medical imaging workflow, transforming raw image data into actionable clinical intelligence.
How AI Is Reshaping the Imaging Workflow

Artificial intelligence is no longer a theoretical concept in healthcare; it is an active co-pilot for clinicians, fundamentally re-architecting the medical imaging workflow. Rather than replacing human expertise, AI serves as an intelligent augmentation layer, enhancing the capabilities of radiologists and technologists at every stage of the diagnostic journey.
This human-machine collaboration is catalyzing a new era of precision and efficiency. AI-driven tools can now analyze innumerable variables—patient history, scanner availability, staffing—to optimize appointment scheduling. This intelligent front-end management minimizes wait times, maximizes resource utilization, and sets the foundation for a frictionless workflow. Its impact deepens profoundly as we move into clinical operations.
Creating Intelligent and Prioritized Worklists
The traditional "first-in, first-out" model for reading studies is obsolete. A routine exam could easily precede a life-threatening one that arrived just moments later. AI shatters this linear paradigm by creating intelligent, clinically prioritized worklists.
AI algorithms can perform a preliminary analysis of images upon arrival in the PACS, automatically flagging studies with suspected critical findings like intracranial hemorrhage or pulmonary embolism. These high-priority cases are instantly escalated, ensuring they receive immediate radiologist attention. This transforms the workflow from a passive queue into a proactive, life-saving system.
This market's explosive growth is a testament to its value. In 2025, the global AI in medical imaging market is valued at USD 1.67 billion and is projected to surge to USD 14.46 billion by 2034. This reflects AI's undeniable impact on enhancing diagnostic accuracy and operational agility. For a more granular view, consult this medical imaging AI market analysis.
By automatically prioritizing urgent studies, AI ensures that the most critical patients receive the fastest attention. This simple shift in the medical imaging workflow can dramatically reduce the time between scan and diagnosis for life-threatening conditions.
Augmenting Diagnostics with a Second Set of Eyes
During interpretation, AI functions as an invaluable diagnostic partner. Computer-aided detection (CADe) algorithms act as a vigilant second reader, meticulously analyzing images for subtle indicators of pathology that might be missed by the human eye, especially during high-volume shifts.
Consider these applications:
- Oncology: An AI algorithm can highlight a sub-centimeter pulmonary nodule on a chest CT, prompting closer scrutiny for early-stage malignancy.
- Neurology: In stroke imaging, AI can rapidly quantify the ischemic core volume, providing clinicians with critical data for time-sensitive treatment decisions.
- Breast Imaging: Sophisticated algorithms are trained to detect suspicious microcalcification clusters in mammograms, often the earliest sign of breast cancer.
These tools do not provide the final diagnosis. They strategically direct the radiologist's attention, thereby increasing diagnostic confidence and improving detection rates. Explore more on how healthcare artificial intelligence is being integrated for a comprehensive overview.
Boosting Operational Efficiency Across the Board
Beyond clinical decision support, AI is a powerful engine for operational efficiency across the medical imaging workflow. Its greatest contribution is the automation of repetitive, time-intensive tasks that contribute to burnout and introduce variability.
For instance, AI can perform automated measurements of tumors and other anatomical structures—a tedious task prone to inter-observer variability. By delivering consistent, reproducible measurements in seconds, AI liberates radiologists to focus on high-value cognitive tasks like complex diagnostic reasoning. For a deeper perspective, this guide on AI-powered workflow automation is an excellent resource.
Ultimately, by orchestrating scheduling, prioritizing worklists, flagging abnormalities, and automating measurements, AI empowers highly trained professionals to dedicate their expertise where it matters most: complex patient care.
Connecting Care with Teleradiology and Cloud Platforms
Geography should never be a determinant of healthcare quality. The traditional model, where a radiologist's expertise was confined to the physical boundaries of their institution, is rapidly becoming obsolete. Today, teleradiology and cloud platforms are dismantling these limitations, creating a connected ecosystem where expertise is democratized and accessible across cities, states, and even continents.
This paradigm shift has profound implications for the medical imaging workflow. It enables a subspecialist in a major academic center to provide a real-time interpretation of a critical CT scan for a patient in a remote, rural hospital. This is not merely a matter of convenience; it is about elevating the standard of care in underserved communities and ensuring 24/7 access to specialized diagnostic insights.
Breaking Down Geographic Barriers
The core technologies driving this transformation are Cloud PACS (Picture Archiving and Communication Systems) and Vendor-Neutral Archives (VNAs). Unlike legacy on-premise servers that silo data within a single facility, these cloud-native solutions establish a centralized, secure, and universally accessible repository for medical images.
An on-premise PACS is akin to a local library, accessible only to those physically present. A cloud platform functions like a vast, global digital library, available from any location with a secure internet connection. This fundamental architectural difference unlocks unprecedented levels of collaboration and operational flexibility.
Facilitating Seamless Collaboration
When images reside in a centralized cloud environment, secure and instantaneous sharing becomes the default. This is a strategic advantage for several key healthcare functions:
- Second Opinions: A local radiologist can seamlessly consult a subspecialist hundreds of miles away on a complex case, enhancing diagnostic certainty.
- Multidisciplinary Teams: A patient’s complete imaging history becomes accessible to their entire care team—surgeons, oncologists, pathologists—regardless of their physical location.
- Workload Balancing: Health systems can intelligently distribute their imaging volume across all available radiologists in their network, eliminating backlogs and optimizing turnaround times.
Cloud platforms transform the medical imaging workflow from a series of isolated, linear steps into a dynamic, interconnected network. It ensures that the right expert is looking at the right images at the right time, no matter where they are.
This evolution toward a distributed diagnostic model is more than an efficiency upgrade. It represents a fundamental democratization of medical expertise, making world-class specialized care accessible to all. By embracing these platforms, healthcare organizations can build a more resilient, responsive, and equitable system for every patient.
Adopting Best Practices for a Secure Workflow

Technological innovation is only one half of a world-class medical imaging workflow. True excellence is achieved when this technology is built upon an unbreachable foundation of security, interoperability, and rigorous regulatory compliance. When handling Protected Health Information (PHI), there is zero tolerance for error.
These best practices are the non-negotiable tenets for fortifying your diagnostic operations. They ensure your workflow is not just efficient, but also robust, legally defensible, and deserving of patient trust. This is about architecting resilience from the ground up.
The Language of Interoperability
For disparate imaging systems, electronic health records, and reporting platforms to communicate, they must speak a common language. Without universal standards, the workflow fractures into isolated data silos, creating operational friction and introducing unacceptable risk.
Two standards form the bedrock of this interconnected landscape:
- DICOM (Digital Imaging and Communications in Medicine): This is the global standard for transmitting, storing, and viewing medical images. It ensures that an MRI acquired on one vendor's scanner can be interpreted flawlessly on another's workstation.
- HL7 (Health Level Seven): This standard governs the exchange of clinical and administrative data. It allows a Radiology Information System (RIS) to seamlessly communicate scheduling data and reports with a hospital's enterprise Electronic Health Record (EHR).
Adherence to these standards is the sine qua non of a modern workflow, ensuring fluid and accurate data exchange across the entire patient journey.
Fortifying Defenses with Cybersecurity
The healthcare sector remains a prime target for cyberattacks, elevating data protection to a board-level priority. A breach is not merely a privacy violation; it can disrupt clinical operations and irrevocably damage patient trust. A multi-layered cybersecurity strategy is therefore essential for any medical imaging workflow.
Protecting patient data is not just an IT task; it is a fundamental component of patient safety. A secure workflow is a prerequisite for delivering high-quality, reliable diagnostic care.
Key defensive measures include granular access controls to enforce the principle of least privilege and end-to-end encryption for all data, both at rest and in transit. Regular, independent security audits are critical for proactively identifying and remediating vulnerabilities. As you architect your security posture, reviewing general principles for data security in a workflow context can provide valuable guidance.
Navigating HIPAA Compliance
In the United States, the Health Insurance Portability and Accountability Act (HIPAA) establishes the legal framework for protecting patient data. Compliance, however, is not a one-time certification; it is a continuous commitment that must be woven into the fabric of daily operations.
This entails conducting regular risk assessments, providing comprehensive and ongoing staff training on privacy rules, and maintaining clear, tested protocols for incident response. By embedding these practices directly into the workflow, compliance becomes the organizational default, ensuring operations are not only efficient but also ethically and legally unimpeachable.
Future-Proofing Your Diagnostic Capabilities
The medical imaging workflow is not a static process; it is a dynamic discipline continually reshaped by technological innovation. To maintain a competitive edge, healthcare organizations must look beyond current standards and strategically prepare for the next generation of diagnostic tools. This requires a forward-thinking approach that expands the very definition of what a diagnostic scan can deliver.
We are transitioning from static, anatomical snapshots to dynamic, multi-layered data streams. We are entering an era where an imaging study provides not just a picture, but a functional and physiological narrative of the human body. This evolution promises to yield more definitive answers and unlock the potential of truly personalized medicine.
The Rise of Multi-Dimensional Imaging
A significant leap forward is the adoption of 4D imaging. Unlike a conventional 3D scan that renders a static anatomical model, 4D imaging incorporates the dimension of time, allowing clinicians to visualize organs in real-time motion.
Imagine observing cardiac valve function or mapping complex blood flow patterns dynamically. This is no longer science fiction; it is a powerful diagnostic paradigm providing unprecedented insight into organ function, not just structure.
This technology is already transforming the management of complex cases. Innovations like 4D Flow MRI, which can capture cardiac blood flow at a temporal resolution of 50 milliseconds, provide cardiologists with the precise hemodynamic data needed to manage conditions like congenital heart disease.
Fusing Modalities for Deeper Insights
Another transformative trend is the growth of hybrid imaging, which integrates the strengths of two distinct scanning technologies into a single, synergistic examination. The most prominent example is PET/MRI, which fuses the metabolic data from Positron Emission Tomography with the superior soft-tissue contrast of Magnetic Resonance Imaging.
By layering functional and anatomical information, hybrid imaging provides a complete diagnostic picture that is far greater than the sum of its parts. It allows clinicians to see not just what a lesion looks like, but how it is behaving biologically.
This fusion has profound implications for oncology and neurology. For instance, advanced PET-MRI systems have demonstrated a 28% reduction in false negatives for prostate cancer biopsies compared to MRI alone.
By delivering this level of precision, hybrid imaging refines the entire medical imaging workflow. It enables earlier, more accurate diagnoses and directly informs more effective treatment strategies. This continuous evolution is pushing the boundaries of diagnostics, leading to more definitive clinical insights and, ultimately, superior patient outcomes.
Got Questions? We've Got Answers
This section addresses the most pressing questions that arise when optimizing the medical imaging workflow, offering a quick-reference guide to clarify key concepts and strategic considerations.
What's the Biggest Bottleneck in a Typical Medical Imaging Workflow? The most significant friction point is almost universally found in the image interpretation and reporting stage.
High caseloads combined with inefficient, manual worklist management can extend report turnaround times from hours to days for non-emergent studies.
- Primary Causes of Gridlock:
- Overburdened radiologist worklists.
- Suboptimal case prioritization and assignment.
- Inefficiencies in report dictation, transcription, and approval.
Intelligent automation offers a powerful solution, minimizing manual sorting and accelerating report generation. For example, the adoption of structured reporting templates has been shown to reduce report variability by over 30%, enhancing clarity for referring clinicians.
How Do RIS and PACS Actually Work Together? The simplest analogy is to view the RIS as the operation's brain and the PACS as its heart.
The RIS (Radiology Information System) manages the workflow's logistical and administrative data—patient demographics, orders, scheduling, and billing. The PACS (Picture Archiving and Communication System) is the repository responsible for the storage, retrieval, and distribution of the images themselves.
One imaging center, for example, reduced data transfer delays by 40% simply by enabling direct, automated messaging between their RIS and PACS.
A Deeper Look at RIS and PACS Integration
When RIS and PACS are seamlessly integrated, patient records and their corresponding imaging studies remain perfectly synchronized. This tight coupling eliminates manual data entry, prevents errors, and ensures images are always linked to the correct order.
In practical terms, this means radiology teams spend less time on administrative reconciliation and more time on clinical interpretation. Advanced integrations can even trigger real-time alerts when new, high-priority images arrive in the PACS.
What’s the Difference Between Teleradiology and a Cloud PACS? This is a common point of confusion. Teleradiology is the clinical practice of radiologists interpreting images from a remote location. Cloud PACS is the enabling technology that makes modern, scalable teleradiology possible by hosting images in a secure, web-accessible environment.
- Why Cloud PACS is a Strategic Imperative:
- It offers infinite scalability to accommodate growing data volumes.
- It provides inherent disaster recovery and business continuity.
- It shifts capital expenditures to a more flexible operational expense model.
A cloud-native architecture provides radiologists with secure, near-instant access to images, which can reduce download times by up to 90%. It also allows facilities to reduce on-site IT infrastructure costs by as much as 50% while simplifying regulatory compliance.
You can't have modern teleradiology without a Cloud PACS. It's the backbone that replaces clunky local servers with scalable, web-based storage that powers global collaboration.
Is AI Going to Replace Radiologists? The definitive answer is no. AI is being developed as a powerful augmentation tool to assist radiologists, not to replace their critical cognitive expertise.
AI excels at narrow, data-intensive tasks like flagging potential abnormalities or performing automated measurements. It functions as a tireless second reader, liberating the human expert to focus on complex differential diagnoses and clinical correlation.
- AI intelligently triages worklists, escalating potentially critical cases.
- AI provides a preliminary analysis for expert human review and validation.
- AI automates measurements, reducing inter-observer variability and saving time.
Clinical teams leveraging AI often report a reduction in interpretive errors by approximately 15%, thanks to these automated quality checks. Furthermore, they see over 25% faster case throughput when AI tools are integrated into their workflow. This powerful human-machine collaboration leads to faster, more confident diagnoses.
Where to Learn More
To continue your exploration, we invite you to access our in-depth guides and industry case studies on the RAD365 blog.
You can also subscribe to our newsletter for executive insights on workflow optimization and emerging technologies.
Ready to architect a more intelligent medical imaging workflow? Discover how RAD365 can empower your organization to streamline processes, enhance diagnostic accuracy, and ensure compliance across the enterprise. Visit RAD365.com to schedule a demo today!
