Radiology workflow automation has evolved beyond a technological upgrade; it now represents a strategic imperative for modern imaging departments. This is not merely about adopting new software but about fundamentally re-engineering the diagnostic journey—from patient scheduling to final report delivery. For forward-thinking leaders, embracing automation is a direct and necessary response to the immense pressures defining contemporary radiology, ensuring both operational resilience and clinical excellence.
The Growing Crisis in Modern Radiology Departments

Imagine an air traffic control tower navigating a blizzard with outdated equipment and a skeleton crew. This analogy is alarmingly close to the reality in many radiology departments today. They are caught in a perfect storm of challenges that seriously threatens their capacity to deliver timely, accurate care. The conversation has shifted from buzzwords like 'burnout' to a frank acknowledgment of a systemic crisis demanding immediate, intelligent intervention.
This crisis is fueled by relentless pressures. Shocking vacancy rates mean fewer radiologists and technologists are left to manage a perpetually expanding workload. Compounding this is a crushing administrative burden, where highly skilled clinicians dedicate precious hours to data entry, scheduling, and other non-interpretive tasks that divert their focus from diagnostic imaging.
Simultaneously, the demand for faster turnarounds on increasingly complex scans has never been higher. A referring physician requires critical diagnostic insight now to inform a life-saving decision, positioning the radiology department at the very nexus of the modern patient care pathway.
The Staggering Impact of Staff Shortages
The strain on radiology teams is amplified by a persistent, widespread talent shortage. As we look towards 2025, automation has become a non-negotiable solution to tackle these challenges head-on. Alarming data reveals that 47.8% of hospitals are contending with vacancy rates exceeding 10%, which translates to fewer clinicians available for patient care. To counteract this, it is projected that by 2025, 80% of healthcare organizations will leverage intelligent automation tools to bridge this critical gap. Further insights on healthcare's adaptation can be found on csicompanies.com.
This staffing deficit creates a dangerous downward spiral. The remaining team members are forced to handle escalating case volumes, which elevates the risk of fatigue and diagnostic errors. The intense pressure makes retaining experienced professionals and attracting new talent increasingly difficult, deepening the crisis.
For industry leaders, the question is no longer if they should adopt new technology, but how quickly they can implement solutions that alleviate this immense pressure on their teams and future-proof their operations.
The Problem of Operational Inefficiency
Beyond staffing, many departments are constrained by outdated, fragmented workflows that create a cascade of bottlenecks. These operational hurdles manifest in several frustrating ways:
- Manual Task Overload: Radiologists and technologists are frequently bogged down by repetitive work, such as manually routing studies, locating prior images, or transcribing dictated reports.
- Communication Gaps: Disjointed communication between schedulers, technologists, radiologists, and referring physicians leads to delays, incorrect exam orders, and diminished patient satisfaction.
- Lack of Prioritization: Without intelligent systems, an urgent case can languish in a queue behind routine studies, delaying a critical diagnosis for a patient in the emergency department.
These inefficiencies do not merely slow operations; they directly erode the quality of care and fuel staff dissatisfaction. Radiology workflow automation emerges not as a mere convenience but as an urgent and necessary solution for these foundational problems, offering a clear strategy to restore balance and elevate outcomes.
What Radiology Workflow Automation Actually Looks Like
Let's clarify a common misconception. When discussing "automation" in radiology, it is easy to envision a single, monolithic solution. The reality is far more sophisticated—and infinitely more valuable.
Think of it less as one tool and more as an intelligent, high-tech orchestration platform for the entire diagnostic journey. Radiology workflow automation is not one piece of software; it's an interconnected ecosystem designed to bring precision and efficiency to every stage. To truly grasp its impact, it is helpful to first understand the core concepts of workflow automation.
This system constitutes the digital backbone that integrates scheduling, image acquisition, radiologist review, and final report distribution into a seamless, continuous operation.
Its primary function is to assume the repetitive, low-value tasks that consume clinicians' time. This includes manual data entry, searching for prior studies, and determining appropriate radiologist assignments. By managing this administrative overhead, automation liberates radiologists and technologists to concentrate their expertise where it matters most: on complex diagnostic challenges and patient care.
From Manual Steps to an Intelligent System
In a traditional setting, the radiology process is a disjointed series of manual handoffs. An order is received, an appointment is scheduled, a technologist performs the scan, and the images are placed in a long, unordered queue for the next available radiologist. Each step represents a potential bottleneck and an opportunity for human error or miscommunication.
Automation transforms this fragmented sequence into a smart, interconnected system.
- Order and Scheduling Automation: The moment a physician places an order, the system can instantly verify it for completeness, flag potential contraindications, and propose an optimal scheduling slot based on machine availability and patient urgency.
- Intelligent Image Routing: Once an image is captured, it is not simply relegated to a general worklist. The system analyzes the exam type and patient history to automatically route it to the radiologist with the correct subspecialty—for instance, directing a brain MRI straight to a neuroradiologist.
- Prioritization of Critical Cases: Emergency cases are automatically flagged and elevated to the top of the queue. This is a transformative capability. It means a suspected stroke or internal bleed is reviewed in minutes, not hours, which can dramatically alter a patient's outcome.
The Real-World Impact on Daily Operations
This shift from manual to automated processes is not just a theoretical upgrade; it delivers tangible improvements that teams experience daily. The goal is to create an environment where technology genuinely supports clinical expertise rather than impeding it.
By intelligently managing the flow of patients, data, and resources, radiology workflow automation acts as the central nervous system for a modern imaging department. It ensures the right information gets to the right person at precisely the right time.
The infographic below illustrates how these efficiencies translate into real benefits, with hard data on reduced turnaround times, increased exam throughput, and a significant reduction in errors.
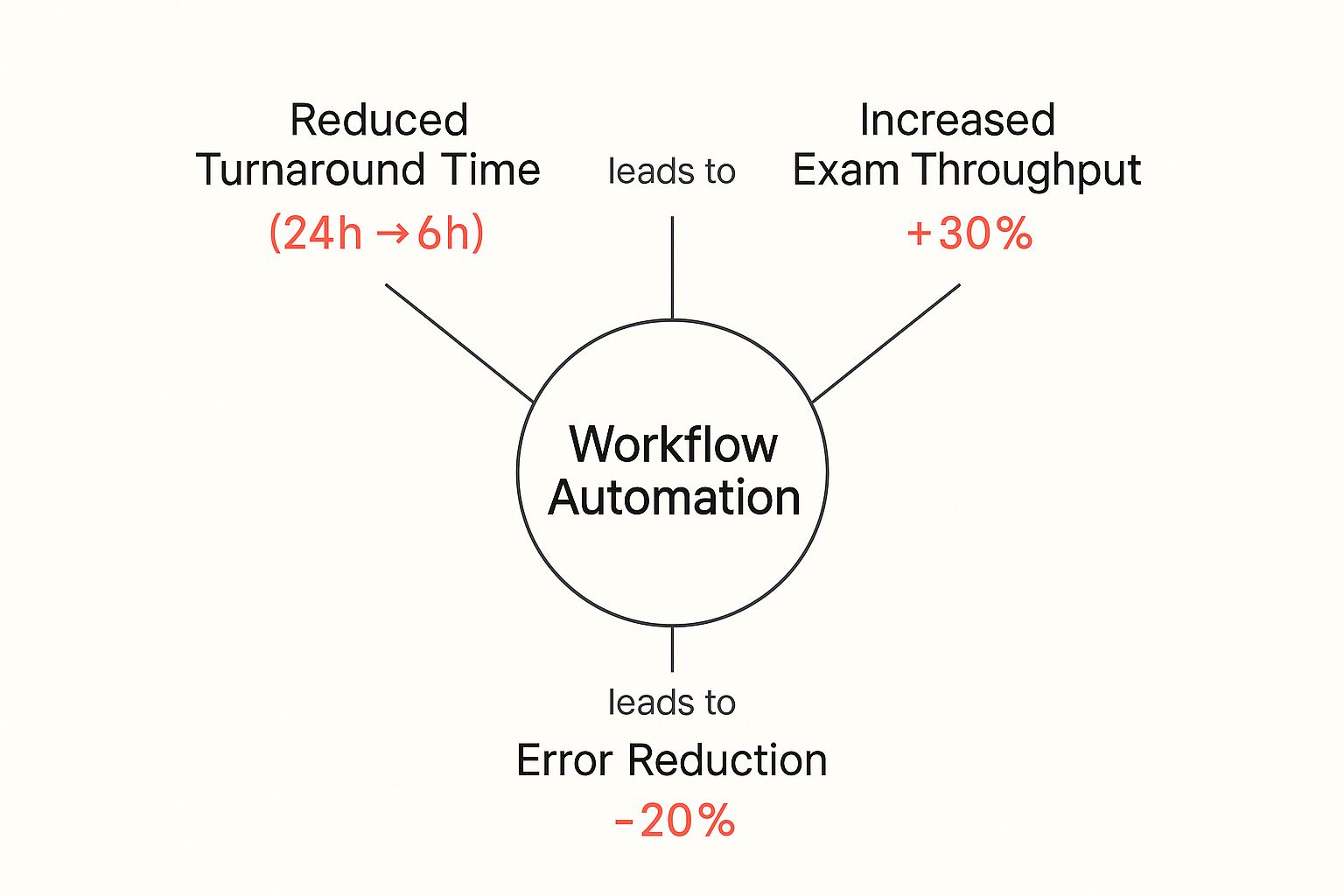
This visual brings these concepts to life, converting abstract ideas into concrete metrics that directly impact both patient care and the financial health of the organization.
Integrating these automated processes is a critical component of modern https://www.rad365.com/healthcare-technologies, which are all geared toward improving clinical outcomes and making operations more resilient. By eliminating bottlenecks and easing the cognitive load on staff, departments can finally manage growing imaging volumes without ever sacrificing quality or speed.
How Automation Delivers Tangible Clinical Benefits

Understanding the mechanics of automation is one thing; witnessing its direct impact on patient care and operational excellence is another. The true value of radiology workflow automation lies not in buzzwords but in the concrete, measurable victories it delivers across the entire diagnostic continuum.
These advantages can be categorized into three core areas: radical efficiency, enhanced diagnostic accuracy, and a profound improvement in patient outcomes. When one link in the chain is fortified, the positive effects cascade throughout the system.
Radical Gains in Operational Efficiency
At its core, automation is an efficiency engine. It targets the small, repetitive tasks that consume a radiologist's day. An intelligent worklist functions like an expert dispatcher, automatically triaging incoming studies by urgency, complexity, and the appropriate subspecialist.
This ensures that a critical head CT from the ER is instantly flagged and moved to the top of the queue, while routine outpatient scans are assigned optimally. This single change can reduce report turnaround times (TAT) for urgent cases from hours to mere minutes.
Once a diagnosis is rendered, automated reporting and distribution tools ensure the findings are immediately delivered to the right hands, eliminating delays.
Enhanced Diagnostic Accuracy and Confidence
Beyond speed, automation introduces a powerful layer of quality control. AI-powered tools function as a tireless second set of eyes, scanning every image for subtle indicators that might be overlooked during a demanding shift. These algorithms are trained to identify patterns associated with specific conditions, highlighting areas for the radiologist's review.
This technology does not replace the radiologist's judgment; it augments it. By drawing attention to potential findings, these tools mitigate perceptual errors and increase clinicians' confidence in their interpretations. This is crucial for reducing cognitive load and upholding a high standard of care, even under intense pressure.
A well-architected automated workflow does more than accelerate processes—it builds in safeguards that elevate the quality and reliability of every single diagnosis, leading to more effective and safer patient care.
This fusion of speed and precision has also facilitated specialized collaboration more than ever before. It is a cornerstone of modern diagnostics, connecting experts across any distance. For a deeper exploration, our complete guide to teleradiology services demonstrates how this synergy works in practice.
The table below details how automation transforms each stage of the radiology process, converting bottlenecks into streamlined operations.
Impact of Automation Across the Radiology Workflow
| Workflow Stage | Manual Process Challenges | Automated Workflow Solution |
|---|---|---|
| Pre-Scan | Manual scheduling and patient data entry lead to errors and delays. | Automated scheduling, pre-registration, and protocoling based on EHR data. |
| Image Acquisition | Technologists spend time on repetitive scanner setup and protocol selection. | AI-driven protocol suggestions and automated image quality checks. |
| Image Routing | Manual assignment of studies to radiologists causes bottlenecks and uneven workloads. | Intelligent worklists automatically triage and assign cases by urgency and subspecialty. |
| Interpretation | Radiologists sift through long lists, search for priors, and perform tedious measurements. | AI flagging of critical findings, automatic retrieval of prior exams, and one-click measurements. |
| Reporting | Manual dictation and report creation is time-consuming and prone to inconsistencies. | Structured reporting templates with auto-populated data and voice-to-text integration. |
| Post-Reporting | Delays in communicating critical results and manual follow-up recommendations. | Automated critical results notification and follow-up tracking for incidental findings. |
As this breakdown shows, the impact is comprehensive, felt from the moment a patient is scheduled to long after the report is signed.
Profound Impact on Staff Well-Being
One of the most significant—and often overlooked—benefits is the positive effect on clinical staff. Burnout in radiology is a serious crisis, fueled by crushing administrative burdens and the relentless pressure to read more, faster.
Automation directly addresses the root causes of this problem by taking over thankless tasks like data entry, image routing, and report formatting. This liberates radiologists and technologists to perform the work they were trained for: interpreting complex cases and consulting with referring physicians.
When clinicians are empowered to work at the top of their licenses, job satisfaction soars, and the department becomes a more attractive place to work. A happier, less stressed team is invariably a more effective one, which translates directly to superior care for every patient.
The Role of AI in Supercharging Your Workflow
If radiology workflow automation is the engine driving a modern imaging department, then artificial intelligence (AI) is the sophisticated navigation system. It is the technology that not only executes tasks but also makes intelligent decisions, transforming a fast workflow into a truly brilliant one. The real strategic advantage emerges when automation and AI converge—this synergy unlocks the greatest gains in efficiency and accuracy.
Consider AI as an expert assistant who reviews every case before it reaches a radiologist. This assistant is tireless and perpetually vigilant. It meticulously pre-analyzes each study, flags potential urgencies, and organizes findings into a concise, actionable summary. This is the core function of AI in radiology: to augment the radiologist's expertise, not to replace it.
This collaboration enables departments to manage escalating imaging volumes with far greater precision. Instead of merely processing studies faster, AI helps ensure the right studies are reviewed by the right expert at the right time.
Intelligent Triage with Computer-Aided Systems
One of the most powerful applications of AI is in triage and prioritization. Two key technologies lead this charge: Computer-Aided Detection (CADe) and Computer-Aided Triage (CADt).
Computer-Aided Detection (CADe): This technology functions as a second set of eyes for the radiologist. CADe algorithms are trained to identify and highlight potential abnormalities, such as suspicious nodules on a chest CT or microcalcifications on a mammogram. It serves as a crucial quality check, reducing the risk of perceptual errors during high-volume reading sessions.
Computer-Aided Triage (CADt): While CADe identifies potential findings, CADt is focused on urgency. These systems instantly analyze incoming studies for life-threatening conditions like stroke, pulmonary embolism, or internal bleeding. When a critical finding is detected, the case is automatically flagged and elevated to the top of the worklist for immediate review.
This instant prioritization is a game-changer in emergency radiology. A patient with a suspected brain bleed no longer waits in a queue; their scan is reviewed in minutes, dramatically improving their prognosis.
From Detection to Actionable Insights
AI’s role extends far beyond flagging images. It automates repetitive yet critical tasks that previously consumed a significant portion of a radiologist's day. AI tools are now widely deployed to automate image sorting, preliminary reads, report generation, and, most importantly, triage.
For example, AI-driven CADe and CADt systems can instantly prioritize emergency cases like suspected fractures and pneumothorax, moving them to the front of the line to accelerate care. These advancements are estimated to reduce diagnostic reporting times by up to 30-40%.
By handling the preliminary analysis and prioritization, AI clears the path for radiologists to apply their deep clinical knowledge to the most complex diagnostic challenges. It transforms their role from data processor to expert consultant.
This intelligent partnership is a core component of modern healthcare. To learn more about how these systems are reshaping medicine, explore our detailed overview of healthcare artificial intelligence. The principles driving these advancements are not confined to medicine; the ongoing "Robotics Evolution Advancing Automation With AI" across various industries offers valuable insights applicable to radiology.
Ultimately, integrating AI into radiology workflow automation creates a system that is not only faster but also safer and more reliable. It adds a layer of intelligent oversight that helps clinicians perform at their absolute best, ensuring that even with growing workloads, the standard of patient care continues to rise. This isn't about replacing human expertise; it's about supercharging it.
How to Implement Your Automation Strategy

Embarking on a technological transformation can feel daunting, but a successful transition to radiology workflow automation is achievable with a clear, strategic roadmap. The objective is not merely to install software but to fundamentally enhance departmental operations. A well-planned implementation sidesteps common pitfalls and ensures maximum return on investment from day one.
The process begins not with technology, but with your people and current processes. Before optimizing a workflow, you must deeply understand it. This requires an honest assessment of your operations to identify the precise friction points that impede your team and impact patient care.
Start with a Comprehensive Workflow Analysis
Before you can streamline anything, you must map it out. Think of this as creating a blueprint of your department's daily operations. The goal is to pinpoint your most significant bottlenecks—those specific stages where delays, errors, and wasted effort consistently occur.
This involves more than passive observation. It means engaging with everyone involved, from front-desk staff and technologists to radiologists and billing specialists. Each individual possesses a unique and valuable perspective on operational strengths and weaknesses.
Focus on these key areas during your analysis:
- Report Turnaround Times (TAT): Measure the time from exam completion to the delivery of the final report to the referring physician. Identify which study types consistently experience delays.
- Resource Utilization: Assess the efficiency of your imaging equipment and staff deployment. Are there periods of underutilization followed by chaotic rushes?
- Manual Task Volume: Quantify the hours your team dedicates to repetitive, non-clinical tasks like data entry, image routing, and sending confirmations. This is often the low-hanging fruit where automation can deliver the most immediate and significant impact.
Secure Buy-In from All Key Stakeholders
A new automation strategy impacts everyone, making stakeholder buy-in non-negotiable. Resistance to change is a natural human response, especially when technology threatens established routines. Proactively address concerns by demonstrating how this transformation will improve the daily work life of each group.
Your stakeholders will have distinct priorities:
- Radiologists: They need assurance that automation is designed to augment their expertise, not replace it. Frame it as a tool to eliminate administrative burdens, allowing them to focus on high-level diagnostics.
- IT Staff: This team is focused on security, data integrity, and system integration. Involve them early to discuss technical requirements, HIPAA compliance, and how the new solution will interface with your existing PACS and EHR.
- Hospital Administrators: Their focus is on ROI, patient throughput, and operational efficiency. Use the quantitative data from your workflow analysis to build a compelling business case that aligns with their objectives.
The most successful implementations are invariably collaborative. When every team member understands the 'why' behind the change and feels their input is valued, adoption shifts from a top-down mandate to a shared strategic goal.
Prioritize Scalability and Seamless Integration
The technology you select today must be prepared for tomorrow's challenges. A scalable solution can accommodate rising imaging volumes or the addition of a new facility without requiring a complete overhaul. Equally critical is interoperability. Your automation platform must integrate seamlessly with your existing Picture Archiving and Communication System (PACS) and Electronic Health Record (EHR).
A solution that creates new data silos or forces clinicians to navigate multiple disparate systems is not a solution—it is a new problem. True automation acts as an intelligent layer that connects your existing systems, creating an uninterrupted flow of information.
Implement a Phased Rollout for Smooth Adoption
Instead of a "big bang" launch that disrupts the entire department, adopt a phased rollout strategy. This approach allows you to introduce new automated processes in manageable increments, minimizing operational chaos and giving your team time to adapt.
For example, begin by automating the triage of ER studies or by implementing structured reporting templates for a single modality. This methodology enables you to gather feedback, resolve any issues on a small scale, and secure early victories. As your team observes the positive impact, their confidence—and enthusiasm—for subsequent phases will grow, paving the way for a successful, department-wide transformation.
Choosing the Right Technology Partner for Your Practice
Selecting the right radiology workflow automation platform is a monumental decision. However, choosing the right technology partner is equally critical for your long-term success.
A powerful platform with inadequate support can quickly become a source of frustration, undermining the very operations you seek to improve. Your partner should be a strategic ally, one who is genuinely invested in your clinical and operational objectives.
Think of it as selecting a co-pilot for your department. You need a partner who understands the high-stakes environment of radiology and is committed to ensuring a smooth journey. This requires looking beyond flashy features and asking the tough, practical questions that reveal a vendor's true commitment.
Essential Questions for Vendor Evaluation
Before committing, your team requires clear, direct answers to several non-negotiable questions. These will help you distinguish a true partner from a mere software vendor. A genuine partnership ensures the technology adapts to your needs, not the other way around.
Begin with the technical fundamentals. Seamless integration is not a luxury; it is a prerequisite.
- Interoperability: How will your platform integrate with our existing PACS, RIS, and EHR? Can you provide case studies of successful integrations with systems comparable to ours?
- Scalability: Our practice is growing, and imaging volumes are increasing. How does your platform scale? What is the process, and what are the associated costs?
- Data Security: What specific measures do you have in place to guarantee robust data security and HIPAA compliance? Detail your protocols for data encryption, access controls, and threat detection.
Beyond the Technology Stack
A partner's value extends far beyond their software's code. Their commitment to your success is often most evident in their support structure and their vision for the future. You need a team that will be there to help you navigate challenges and maximize your return on investment.
Choosing a vendor is a long-term commitment. Prioritize partners who demonstrate a deep understanding of clinical workflows and offer responsive, expert support. A cheap solution with unreliable service is no solution at all.
Finally, investigate their forward-thinking capabilities. Does the platform include advanced analytics dashboards to track key performance indicators? What are their AI capabilities, and what is on their roadmap for future AI development? A partner focused on continuous innovation ensures your investment remains valuable for years to come, keeping your practice at the forefront of diagnostic excellence.
Got Questions About Radiology Automation? We've Got Answers.
When considering a significant operational shift like implementing radiology workflow automation, questions are inevitable. This is a major strategic decision, and obtaining clear answers to the most common concerns is the first step toward informed leadership.
Will AI and Automation Replace Radiologists?
This is the most prominent question, and the answer is an unequivocal no.
The strategic purpose of automation and AI in this context is augmentation, not replacement. These tools should be viewed as hyper-efficient co-pilots. They manage routine, repetitive tasks—such as organizing worklists, triaging studies, or performing standardized measurements—freeing the radiologist to concentrate on what truly requires human expertise: complex interpretation, critical thinking, and collaborative patient care.
These systems absorb the administrative burden, which in turn elevates the radiologist's role. It allows them to apply their expertise where it is most impactful, enhancing diagnostic quality and combating the burnout that results from being mired in operational minutiae.
How Does Automation Fit With Our Existing Systems?
A new tool that creates new problems is not a solution. This is why seamless integration is a non-negotiable requirement.
Modern automation platforms are architected to interoperate with your existing technology stack. They utilize industry standards like HL7 and DICOM to communicate with your Picture Archiving and Communication System (PACS), Radiology Information System (RIS), and Electronic Health Record (EHR).
The best solutions act as an intelligent layer that sits on top of your current infrastructure. They pull data from your systems and push updates back in, all without forcing you into a costly and disruptive "rip and replace" of the tools your team already knows.
Always prioritize vendors who can provide demonstrable proof of successful integrations with systems analogous to yours. This is the key to a smooth implementation where benefits are realized immediately.
What Is the Typical Return on Investment?
The ROI for radiology workflow automation extends far beyond simple cost reduction. It is a multi-layered benefit that positively impacts your finances, operations, and—most critically—your clinical outcomes.
- Financial ROI: This is driven by pure efficiency. Radiologists can accurately interpret more studies in the same amount of time, and automated processes result in cleaner billing cycles with fewer errors.
- Operational ROI: Practices experience a dramatic reduction in report turnaround times. Equally important, overall staff productivity and job satisfaction receive a significant boost as frustrating manual tasks are eliminated.
- Clinical ROI: This is where the ultimate value lies. Delivering critical findings to referring physicians faster leads directly to quicker treatment decisions and improved patient outcomes.
Many practices report seeing measurable improvements within months, making this one of the most intelligent strategic investments an organization can make for long-term growth and superior patient care.
At RAD365, we build advanced telehealth and teleradiology solutions designed to empower healthcare providers. Our technologies integrate seamlessly into your current workflows to enhance efficiency and improve patient outcomes. Discover how our solutions can make a difference in your practice at rad365.com.
