What, precisely, is a radiology workflow solution?
Envision it as the central command for a medical imaging department. It's a sophisticated, integrated digital framework that directs and synchronizes every stage of the imaging lifecycle—from initial patient scheduling to the delivery of a definitive, actionable report to the clinician. These solutions represent the operational architecture essential for maintaining the velocity and precision of modern diagnostics.
What Are Modern Radiology Workflow Solutions?

Not long ago, radiology departments operated through a sequence of disjointed, manual processes: paper requisitions, incessant phone calls, and redundant data entry. This legacy model was inefficient and fraught with potential for error. Today, modern radiology workflow solutions have superseded this fragmented approach with a singular, cohesive digital ecosystem.
This is not a single piece of software but rather the central nervous system connecting an array of specialized tools. Its primary mandate is to orchestrate the seamless flow of patients, data, and tasks among all stakeholders. This includes the referring physician, administrative staff, technologists, and, critically, the radiologists themselves.
The Journey of an Image
To fully grasp its impact, let's trace the journey of a medical image. It begins with a physician's order. This triggers scheduling and patient preparation, followed by the image acquisition by a technologist. The images are then processed, archived, and intelligently routed to the appropriate radiologist for interpretation. Finally, a diagnostic report is created, validated, and transmitted back to the referring physician.
A modern workflow solution manages this entire continuum, automating handoffs and ensuring information is precisely where it needs to be at the exact moment it is needed. This automated orchestration is the defining characteristic that elevates modern solutions above the rudimentary systems of the past.
A well-architected radiology workflow functions as a powerful engine, driving productivity, minimizing waste, and ensuring clinicians possess critical information precisely when needed. It transforms a complex series of disjointed steps into a streamlined, cohesive process.
Beyond Basic Task Management
The objective, however, extends beyond mere task delegation. Advanced radiology workflow solutions are engineered to optimize the entire clinical operation. This focus on optimization is non-negotiable in today’s high-volume healthcare landscape, where the demand for diagnostic imaging is relentless.
These systems are mission-critical for:
- Reducing Errors: By automating data entry and standardizing protocols, the risk of human error is substantially mitigated.
- Improving Efficiency: They identify and eliminate bottlenecks, ensuring high-cost imaging equipment is maximally utilized and patient wait times are minimized.
- Enhancing Communication: Integrated platforms facilitate clear, instantaneous communication between radiologists and referring physicians, which is vital for conveying urgent findings.
Ultimately, these systems are no longer a discretionary investment. They are a core strategic component for any imaging department committed to delivering high-quality, timely patient care within a demanding and complex medical environment.
The Core Systems of an Optimized Workflow
At the heart of any high-performing radiology department lies not a single monolithic application, but a digital toolkit—a suite of interconnected systems operating in concert. To truly understand modern radiology workflow solutions, one must look beyond the acronyms and appreciate the distinct functions these core components perform. Each system is a specialist; their collaboration transforms a fragmented process into a seamless operational flow.
This synergy is not merely a matter of convenience; it yields significant operational dividends. A finely tuned workflow translates directly into superior, faster patient care.
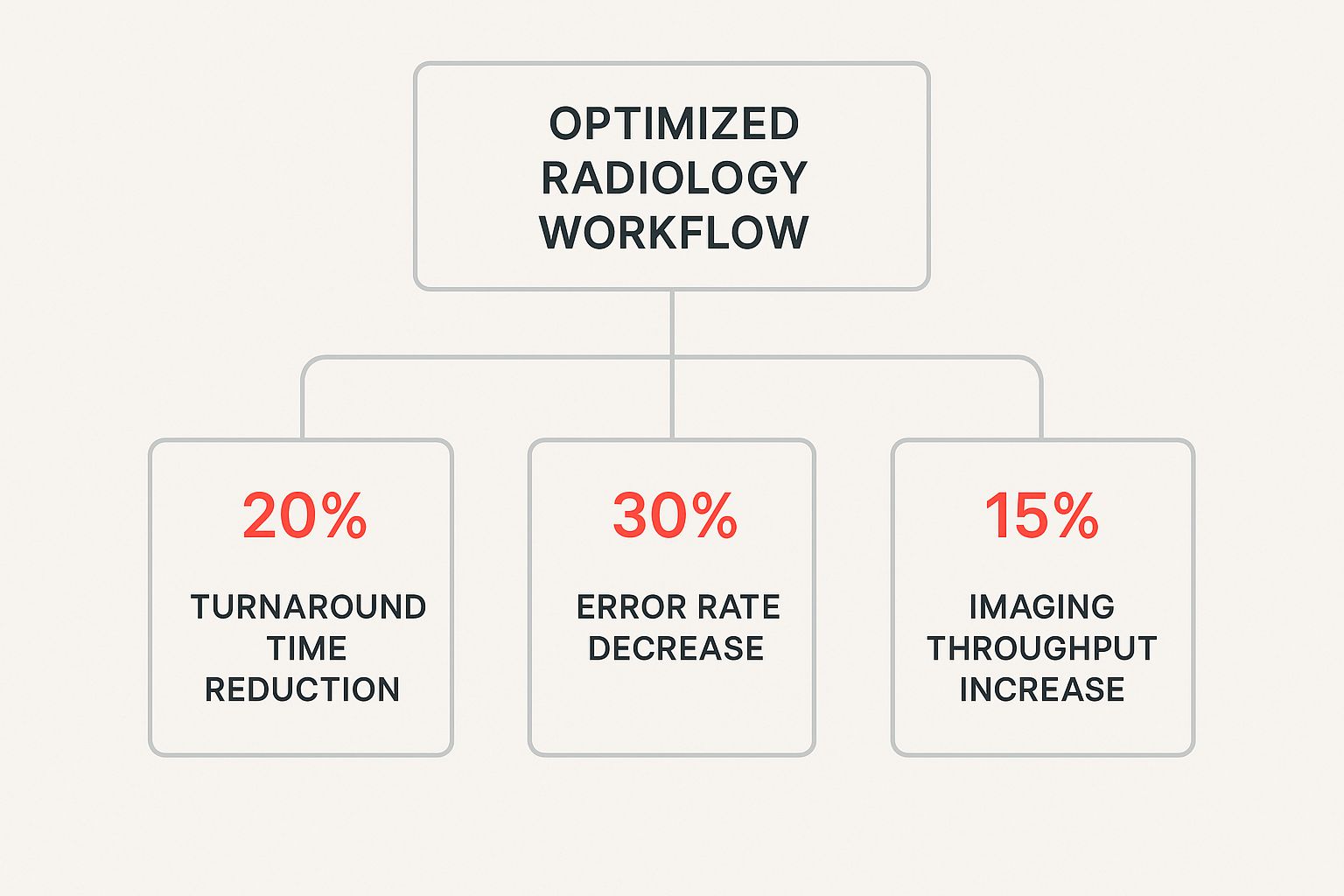
As the data illustrates, strategic technology investment leads to faster diagnostics, reduced error rates, and increased patient throughput. It is a clear win for both providers and patients.
Let's dissect the key players in this digital ecosystem.
Key Systems in a Radiology Workflow Solution
To see how these individual parts create a powerful whole, it is crucial to understand what each system contributes. The table below outlines the three primary components, their core function, and their direct impact on the day-to-day workflow.
| System Component | Primary Function | Impact on Workflow |
|---|---|---|
| Radiology Information System (RIS) | Manages all administrative and operational data surrounding an imaging study. | Acts as the project manager. Orchestrates scheduling, billing, and patient tracking to maintain departmental velocity. |
| Picture Archiving and Communication System (PACS) | Stores, retrieves, and displays all medical images for radiologist interpretation. | Serves as the digital reading room. Empowers radiologists with the tools to view and analyze scans from any modality. |
| Vendor Neutral Archive (VNA) | Provides a standardized, long-term storage solution for images from any vendor system. | Functions as the universal translator. Dismantles data silos, simplifies image exchange, and future-proofs the archive. |
Each system has a specialized role, but their true power is unleashed through their interoperability, creating a single, authoritative source of information for every patient's imaging journey.
The Project Manager: RIS
First is the Radiology Information System (RIS). The most effective way to conceptualize the RIS is as the department's highly organized project manager or central command. While it does not manage the images themselves, it governs all the critical metadata surrounding them.
The RIS performs the logistical heavy lifting. Its responsibilities include:
- Patient Scheduling: Managing appointments, equipment availability, and patient demographics.
- Billing and Coding: Ensuring procedures are coded correctly for accurate reimbursement.
- Patient Tracking: Monitoring a patient's progress from check-in through to report finalization.
- Reporting: Generating analytics on everything from patient throughput to departmental performance metrics.
In essence, the RIS ensures the right patient receives the right scan at the right time.
The Secure Digital Library: PACS
Next is the Picture Archiving and Communication System (PACS). If the RIS is the project manager, the PACS is the vast, secure digital library where every medical image is archived. Its entire purpose revolves around image management.
This is the system where radiologists conduct the majority of their work. It provides them with the tools to instantly retrieve, display, and interpret scans from X-rays, CTs, and MRIs. A robust PACS also offers advanced visualization tools like 3D rendering and facilitates comparison with prior studies—a crucial step for accurate diagnosis.
The Universal Translator: VNA
Finally, we have the Vendor Neutral Archive (VNA). Imagine a library where each book is written in a different, proprietary language, making information sharing impossible. The VNA serves as the universal translator, ensuring that medical images can be accessed and interpreted by any system, regardless of the vendor that created them.
A VNA effectively decouples the images from the PACS in which they were originally stored. This is a game-changer for long-term data stewardship, allowing a hospital to switch PACS vendors without the monumental challenge of migrating petabytes of historical imaging data. It also streamlines the sharing of images between different healthcare institutions, fostering a more unified patient record.
The real power isn’t in any single system but in their fluid communication. When the RIS, PACS, and VNA are perfectly integrated, they create a single source of truth for every patient's imaging journey, effectively breaking down data silos.
A cornerstone of any modern workflow is effective system integration, which ensures all these platforms communicate seamlessly. When a radiologist opens a study in the PACS, the corresponding patient data and report from the RIS should appear automatically. This connected ecosystem is the secret to efficient and accurate diagnostic imaging, a concept we explore further when discussing teleradiology services and specialists in our complete guide for imaging centres.
How AI Is Transforming Radiology Workflows

Artificial intelligence is no longer a futuristic concept in medicine; it is a practical, powerful tool being integrated directly into today’s radiology workflow solutions.
The objective is not to replace the radiologist. On the contrary, AI should be viewed as an exceptionally capable and tireless co-pilot, managing monotonous, time-intensive tasks to liberate the human expert for what they do best: complex diagnostic reasoning and clinical judgment.
This human-machine collaboration is fundamentally reshaping imaging departments, enhancing both the velocity and precision of diagnostics by automating the burdensome work.
Automating the Repetitive to Elevate Expertise
One of the most immediate benefits of AI is its capacity to automate tasks that, while essential, create significant drag on the diagnostic process.
Radiologists historically spent considerable time on manual measurements, such as tracking a lesion's dimensions across multiple scans to assess treatment efficacy. An AI algorithm can now execute these measurements in seconds with superhuman precision.
This automation is creating value in other critical areas as well:
- Lesion Detection: AI can screen thousands of images, flagging subtle anomalies that a human eye might overlook, particularly at the end of a long shift.
- Image Segmentation: It can precisely delineate organs or pathologies, generating a clear roadmap for surgeons or radiation oncologists.
- Report Generation: AI tools can draft preliminary reports by populating standard findings, allowing radiologists to review, amend, and finalize them in a fraction of the time.
These capabilities directly address the pervasive issue of radiologist burnout by offloading the cognitive burden of repetitive tasks.
The true value of AI in radiology isn't just speed; it's about creating a more intelligent, proactive, and sustainable diagnostic environment. It elevates the radiologist's role from data processor to expert interpreter and clinical consultant.
Creating Smarter, Proactive Workflows
Beyond task automation, AI is fundamentally altering the logic of the radiology workflow. It introduces a layer of intelligence that shifts the entire process from reactive to proactive. Instead of images simply accumulating in a worklist, AI-driven systems can analyze incoming studies and prioritize the most urgent cases.
Consider an algorithm that screens a chest X-ray and instantly identifies signs of a pneumothorax. That case is immediately escalated to the top of the queue for review. This intelligent triage means critical findings are addressed in minutes, not hours—a time difference that can be life-saving.
By 2025, initiatives like SPARK Radiology's launch of SPARK.ai demonstrate how rapidly AI-powered solutions are improving report turnaround times and diagnostic accuracy. While regulations are still evolving, many healthcare providers are aggressively adopting AI because the gains in workflow and quality are too significant to ignore. To see how these concepts can be applied more broadly, it's worth learning how to optimize workflow across your organization with AI.
The Future Is Collaborative
The successful implementation of healthcare artificial intelligence is predicated on this human-machine partnership. Radiologists provide the indispensable clinical context, ethical oversight, and nuanced judgment that a machine cannot replicate.
AI, in turn, contributes the raw computational power to analyze massive datasets, identify subtle patterns, and streamline operations at a scale previously unimaginable. This synergy results in a more efficient, accurate, and resilient radiology department, prepared to meet the ever-increasing demand for diagnostic imaging. You can learn more about the broader applications of healthcare artificial intelligence in our detailed article.
The Real-World Benefits of a Modern Workflow
Implementing a modern radiology workflow solution is far more than a technology upgrade; it is a strategic initiative that delivers tangible, measurable results across the entire organization. The true value is not found in technical specifications but in the powerful return on investment reflected in operations, clinical outcomes, and financial performance.
By moving beyond outdated, manual processes, you unlock a new tier of operational excellence. Let’s examine the concrete advantages across three key pillars.
Operational Excellence and Efficiency
From an operational perspective, a streamlined workflow is analogous to replacing congested city streets with a direct superhighway. The immediate impact is a dramatic reduction in friction and wasted time, empowering your department to become more productive and responsive.
Optimized scheduling systems, for instance, maximize the utilization of high-cost MRI and CT scanners, minimizing idle time. This enhanced throughput allows more patients to be seen without additional capital expenditure.
Automation also absorbs the tedious administrative tasks that create bottlenecks, freeing staff to focus on higher-value activities. This directly improves key performance indicators:
- Shorter Patient Wait Times: Automated check-ins and intelligent scheduling move patients through the system more efficiently, significantly enhancing their experience.
- Faster Report Turnaround: By automating image routing and report distribution, the time from scan to diagnosis can be drastically reduced. Some facilities have compressed their average reporting time from 24 hours down to just 4 hours.
- Elimination of Redundant Work: Integrated systems eradicate manual data re-entry, which not only saves time but also mitigates the risk of human error.
Enhanced Clinical Outcomes
The clinical benefits are where the impact becomes most critical. A modern workflow equips radiologists with the tools necessary to deliver more accurate and timely diagnoses—the cornerstone of exceptional patient care.
Advanced communication tools are a prime example. When a radiologist identifies a critical finding, an integrated system can trigger an immediate, automated alert to the referring physician, eliminating the communication delays that can jeopardize patient safety. For a deeper look at how this plays out, this case study on the importance of a second opinion provides valuable insights.
The core clinical advantage of an optimized workflow is creating an environment of certainty. It ensures the right information gets to the right specialist at the right time, minimizing ambiguity and accelerating the path to treatment.
AI-powered tools also function as a second set of eyes, augmenting the radiologist's expertise. These systems can triage worklists to prioritize urgent cases or flag subtle abnormalities for closer examination, providing a crucial safety net that enhances diagnostic confidence and improves patient outcomes.
Stronger Financial Health
Finally, the financial return from a modern workflow is undeniable. By making a practice more efficient and accurate, radiology workflow solutions directly contribute to a more robust financial position.
Automation reduces operational costs by minimizing the manual labor required for scheduling, billing, and records management. Billing accuracy is also significantly improved. When the Radiology Information System (RIS) communicates directly with the billing platform, procedure codes are captured correctly at the source, resulting in fewer claim denials and a more streamlined revenue cycle.
It is no surprise that the medical imaging and radiology software market, valued at $7.35 billion in 2024, is projected to reach $11.09 billion by 2029. This growth, detailed in recent market analysis on radiology software trends, is a clear indicator that healthcare providers are realizing significant financial and operational benefits.
Choosing and Implementing Your Solution
Implementing a new radiology workflow solution is a significant undertaking. It is not merely a software acquisition but a fundamental transformation of departmental operations. This requires a disciplined, strategic plan to ensure you select the right vendor and guide your team through a successful transition.
Success is not determined at contract signing. It begins with a rigorous and honest assessment of your current state and the establishment of clear, strategic objectives.
Assess Your Current State and Define Clear Goals
Before evaluating any solution, you must develop a detailed understanding of your existing workflow—its strengths, weaknesses, and inefficiencies. This is akin to performing a diagnostic on your own operations. Begin by identifying the specific bottlenecks that impede performance.
Are report turnaround times unacceptably long? Is scheduling a source of constant friction? Where do communication gaps exist between technologists and radiologists?
This assessment must be a collaborative effort. Engage radiologists, IT specialists, technologists, and administrators to gain a comprehensive, 360-degree perspective. Once you have identified the pain points, you can establish clear, quantifiable goals for the new system.
These goals must be specific and measurable:
- Reduce average report turnaround time by 30% within the first six months.
- Decrease patient no-show rates by 15% through automated communication.
- Eliminate 95% of manual data entry between the RIS and EMR.
- Improve radiologist satisfaction scores related to workload management.
With these concrete targets, your focus shifts from simply buying software to acquiring a solution that addresses your department's most critical challenges.
Evaluating Vendors on What Truly Matters
The market for radiology workflow solutions is crowded, with every vendor promising transformative results. It is incumbent upon you to look past the sales demonstrations and evaluate potential partners against criteria that predict long-term success.
This market is expanding for a reason—diagnostic demand is increasing, and imaging technology is advancing rapidly. The global radiology market was valued at approximately $33.52 billion in 2024 and is projected to reach $83.42 billion by 2033. This growth is propelled by innovations like AI-powered tools that integrate data across disparate systems, which makes your vendor selection all the more critical. You can explore the data and find more insights on this market growth on datamintelligence.com.
Choosing a vendor isn't just about the technology. It's about starting a long-term partnership. Their reliability, support, and vision for the future matter just as much as the features they offer today.
Focus your evaluation on these non-negotiable criteria:
Seamless Interoperability: Can the solution integrate flawlessly with your existing EMR, PACS, and billing systems? Poor interoperability simply creates new data silos and operational friction. Demand to see case studies and speak with clients who have a similar IT infrastructure.
Scalability and Future-Proofing: Your imaging volume will inevitably increase. The system must be able to scale with you without performance degradation. Inquire about their product roadmap—are they innovating with new technologies like AI and cloud analytics, or are they defending a legacy platform?
Robust Training and Support: How will they facilitate a successful implementation? Look for comprehensive training programs tailored to different roles (radiologists, techs, admins) and a support organization that is responsive, expert, and available 24/7.
Managing the Implementation Journey
The implementation phase is where strategic planning translates into reality. The most common mistake is to treat this as a simple IT project. It is a change management initiative that requires comprehensive buy-in.
Data migration is often the most complex technical component. Collaborate closely with your vendor to develop a detailed plan for migrating patient data and prior images securely and with full integrity.
Simultaneously, focus on your people. Training must be hands-on, role-specific, and ongoing. Designate "super-users" within each department—technically adept individuals who can serve as go-to resources for their colleagues. This peer support is invaluable for building confidence and driving adoption from day one. When you involve your team early and consistently, they transition from being passive recipients of change to active stakeholders in the new system's success.
Common Questions About Radiology Workflows
Exploring radiology workflow solutions invariably raises critical questions from department heads, IT leaders, and clinicians. Understanding implementation, patient impact, and core technology is essential for a successful transition.
Here are some of the most common inquiries, with direct and clear answers.
What Is the Biggest Challenge During Implementation?
The greatest challenge is rarely the technology itself; it is the human element. Securing genuine buy-in from every stakeholder—radiologists, technologists, IT specialists, and administrative staff—is paramount. Without it, even the most advanced software will fail to deliver its promised value.
Achieving this requires a multi-faceted approach:
- Go Beyond Basic Training: A single webinar is insufficient. Provide role-specific, hands-on sessions that demonstrate precisely how the new system improves each individual's daily work.
- Communicate the "Why": Articulate the strategic rationale behind the change. Constantly connect the new workflow to tangible benefits: reduced administrative burden, faster diagnoses, and improved patient outcomes.
- Use a Phased Rollout: A "big bang" implementation invites chaos. A gradual, well-planned rollout allows teams to adapt, builds confidence, and simplifies troubleshooting.
Another significant hurdle is ensuring seamless interoperability with existing systems, particularly the EMR. Creating new data silos or inefficient workarounds is a recipe for failure.
How Do These Solutions Directly Improve Patient Care?
Radiology workflow solutions exert a direct and profound impact on patient outcomes through several key mechanisms.
First, they significantly reduce the time from image acquisition to diagnosis. By automating scheduling and intelligently routing studies, patients receive their results faster. This enables referring physicians to initiate treatment sooner, which is critical in time-sensitive clinical scenarios.
Consider the impact of AI-powered triage, which can automatically flag urgent findings for immediate review. This transforms the worklist from a simple "first-in, first-out" queue to a dynamic one based on clinical acuity. This represents a monumental leap forward in patient safety.
These systems also eliminate critical communication gaps. Integrated tools ensure that referring physicians receive clear, accurate, and actionable reports promptly, preventing the delays that can compromise patient care.
Can Smaller Imaging Centers Benefit from These Solutions?
Absolutely. In fact, modern, cloud-based workflow platforms are a transformative force for smaller practices. They democratize access to sophisticated tools that were once the exclusive domain of large hospital networks, leveling the competitive playing field without the prohibitive cost of on-premise servers and hardware.
For smaller centers, the advantages are immense:
- They can leverage teleradiology and AI capabilities to expand their service offerings.
- By automating administrative tasks and optimizing schedules, clinics can increase patient throughput with existing staff.
- They reduce operational overhead, freeing up capital for investment in patient-facing technologies.
By adopting these solutions, smaller practices can not only survive but thrive, competing on quality and efficiency to deliver superior service to their communities.
What Is the Core Difference Between a RIS and a PACS?
This is a fundamental question, and an analogy is often the clearest way to explain it. Think of the RIS as the "brain" of the imaging department and the PACS as its "eyes and library."
The Radiology Information System (RIS) is the logistics manager. It governs all the data surrounding the images:
- Scheduling patient appointments
- Tracking patient status throughout the department
- Managing billing and insurance information
- Generating reports on operational metrics
The Picture Archiving and Communication System (PACS), conversely, is exclusively focused on the images themselves. It is the repository where scans are stored, retrieved, and viewed. Radiologists operate primarily within the PACS, using its specialized tools to analyze images and formulate a diagnosis.
A superior radiology workflow solution functions as the connective tissue between these two systems, ensuring they are perfectly synchronized. It automatically links the correct patient data from the RIS to the corresponding images in the PACS, eliminating errors and saving valuable time.
At RAD365, we specialize in providing advanced teleradiology services and AI-powered solutions that integrate seamlessly into your existing workflow, enhancing efficiency and improving patient outcomes. Discover how our technologies can optimize your operations by visiting us at https://www.rad365.com.
